85 years old
CFS 3
4AT 12
NEWS 0
Pneumonia. AKI. Delirium
85 years old
CFS 7
4AT 3
NEWS 0
Pneumonia
Two short stories. Both just 5 lines long
Do they mean anything to you?
For me as a trained observer, there is tension and drama as the lines are being read out
CFS 3
4AT 12
What?
This is a case of delirium. 4AT 12? A severe one. The patient may not be talking. They may be very drowsy or markedly hyperactive. But why? CFS 3 suggests they normally look after themselves. They go to the shops, clean the house. More than that, they haven’t slowed down. They are independent.
Yet right now, they may be lying unconscious in bed
NEWS 0?
Someone can lie unconscious with a NEWS of 0? I’m doing shortcuts in my brain. Most commonly this kind of presentation might be a severe infection, with AKI, maybe a drug accumulation of something like an opioid.
But also, maybe a stroke? Subdural? Non-convulsive status? And lots of things in between.
“Pneumonia, AKI, Delirium”
Ok makes more sense to me now. I really want to look at their drugs. And yes, they are (still) on a buprenorphine patch. Can we do a bladder scan? 900 mls? Yikes. Catheter to relieve the distress associated with urinary retention that can cause or contribute to delirium.
Are they eating enough? Are they in pain? Fluids? Bowels? Can family support?
This is what I see and do every day. This is a previously independent person who is sick with a reversible illness. I am not saying we are going to reverse 100% of these illnesses but we can certainly try for those people that want us to try.
But yet, I later read the notes and I read the review “Very frail…”
You wouldn’t take a picture of yourself ill in bed with a pneumonia, in hospital pyjamas and use it for a social media profile, would you? It’s not just not your best self. It’s not your self.
Likewise, we shouldn’t judge someone’s frailty based upon what they look like ill with a pneumonia and AKI and delirium and opioid accumulation. We need a reliable collateral history. The end of the bedogram is not reliable.
This person is not very frail.
They are very ill.
On my inpatient ward, we have fully embraced the GIRFT triple assessment of CFS, 4AT and NEWS 2. I am making my way around our permanent nursing staff to help them understand what these assessments mean, and our doctors are on board. The therapists led the way. When we present cases at our daily MDT, we present them almost exactly in this way. What their CFS and 4AT is and what is wrong with them right now.
I look after half the ward, so I know half the patients well. For the other half, presenting the information in this way is invaluable. If I need to review a patient or provide some specific input then of course I need more detail, but otherwise, in just a few seconds at the beginning of their MDT presentation I get a rich picture of someone’s baseline function, their current cognitive status, whether or not the treating clinician thinks they have a delirium, and the beginnings of what we might need to do to restore them to health.

CFS 7
4AT 3
NEWS 0
Pneumonia
A different story. CFS 7 This is someone with severe frailty. Dependent for most activities of daily living. I wouldn’t expect them to live alone without support. They may have carers multiple times a day, equipment at home. They may live in a care home. They may have very supportive family.
4AT 3. This is someone getting lots of questions on the 4AT wrong.
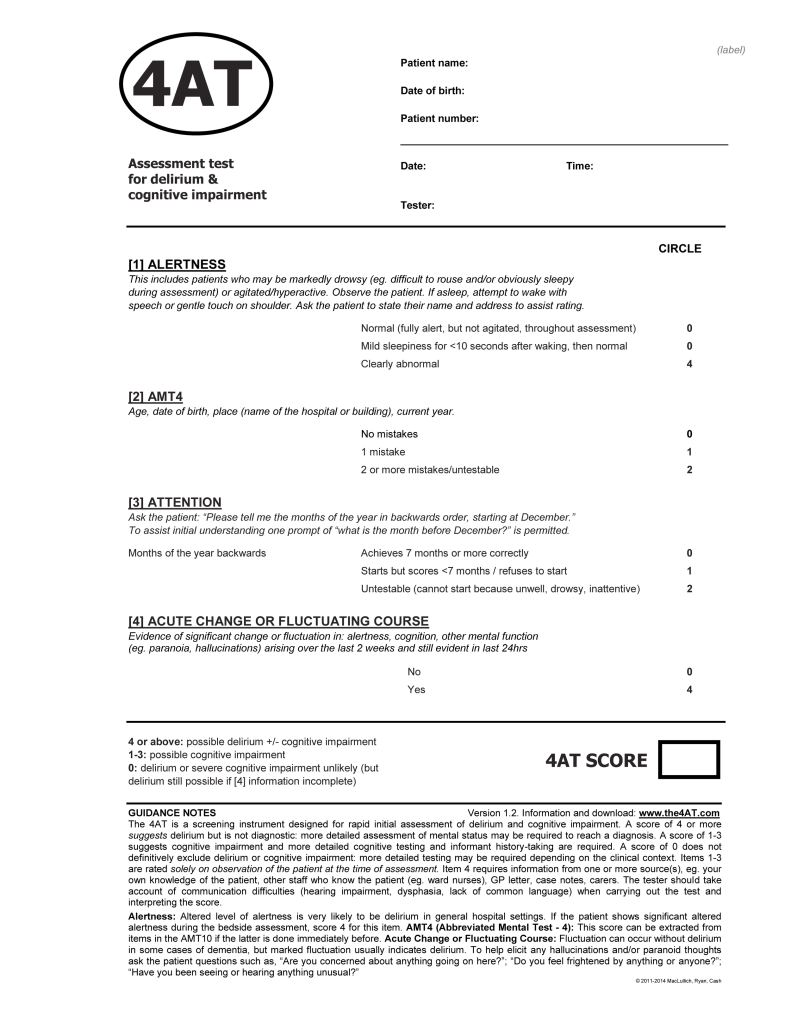
There are only a few ways you might score 3. You must have no acute change and have normal levels of alertness because both of these score 4 when positive.
You have either scored 1 (1 mistake) or 2 for AMT 4 (2 mistakes or more, or untestable) and for months of the year backwards:
1 (refuse to answer, or fail to get to June) or 2 (too inattentive to follow the question) for attention.
When you assess 4AT multiple times a week, you quickly get a sense of what someone with a 4AT of 3 is like. They don’t have delirium, yet they may not know where they are, how old they are, what year it is and they may struggle to follow complex pieces of information.
They may well have dementia (although please don’t assume this). They are certainly at risk of delirium and deconditioning. I think (and one day, I will hopefully get the data to prove it) that this story’s intro is one of the common on my ward.
And while this patient might well be at risk of adverse outcomes, there is also a fair chance that they are not that unwell and may get home soon, despite their apparent dependency and “confusion” on the ward. It’s the sort of person that the untrained observer may be very nervous about sending home, and yet, if they are not ill, no different to their normal selves, not requiring hospital treatment, then really we should be considering getting this person home despite what they just look like without any context.
It’s taken me five years as a consultant to try this. But it’s so obvious. The triple assessment is definitely of benefit, to experts and novices alike. It gives us a framework, and a common language. The clinical frailty scale makes us see that two 85 years olds may be very different in their intrinsic capabilities. The 4AT makes us consider the importance of cognition and delirium. When these are issues we can address them. And it helps us plan, for now, and for tomorrow and the future. With the same illness, one person could go straight home. Another one might need comprehensive geriatric assessment and rehab. Another one still, consideration of end of life care. We teach more on all of this on our course, next available in April 2024.
Short stories. They may have similar middles. But if we use the CFS and 4AT to write the beginning properly, we can better prepare for their ends.